Fill Your Hawaii Polst Template
In Hawaii, the Provider Orders for Life-Sustaining Treatment (POLST) form serves as a critical tool for patients and healthcare professionals, fostering clear communication regarding a patient's preferences for life-sustaining treatments based on their current medical condition and wishes. The form, which should be completed with dignity and respect for every individual, is designed to ensure that the specified medical care aligns with the patient's desires, especially in severe medical scenarios where the patient might be unable to communicate their wishes. Sections of the form cover various areas, including decisions about cardiopulmonary resuscitation (CPR), the extent of medical interventions like comfort measures, limited interventions, and full treatment, and preferences regarding artificially administered nutrition. It also outlines the obligations regarding discussions with the patient or their legally authorized representative (LAR) and the necessity of signatures from the healthcare provider and the patient or LAR to validate the form. The POLST form highlights the importance of transferring the form with the patient whenever they are transferred or discharged, and it upholds the Health Insurance Portability and Accountability Act (HIPAA) permissions for disclosing POLST information to other healthcare professionals as required. Moreover, the POLST form encourages ongoing discussion and reassessment of the patient's wishes, particularly when there is a significant change in the patient's health status or care setting, and it offers guidance on modifying or voiding the form if the patient's treatment preferences change.
Document Example
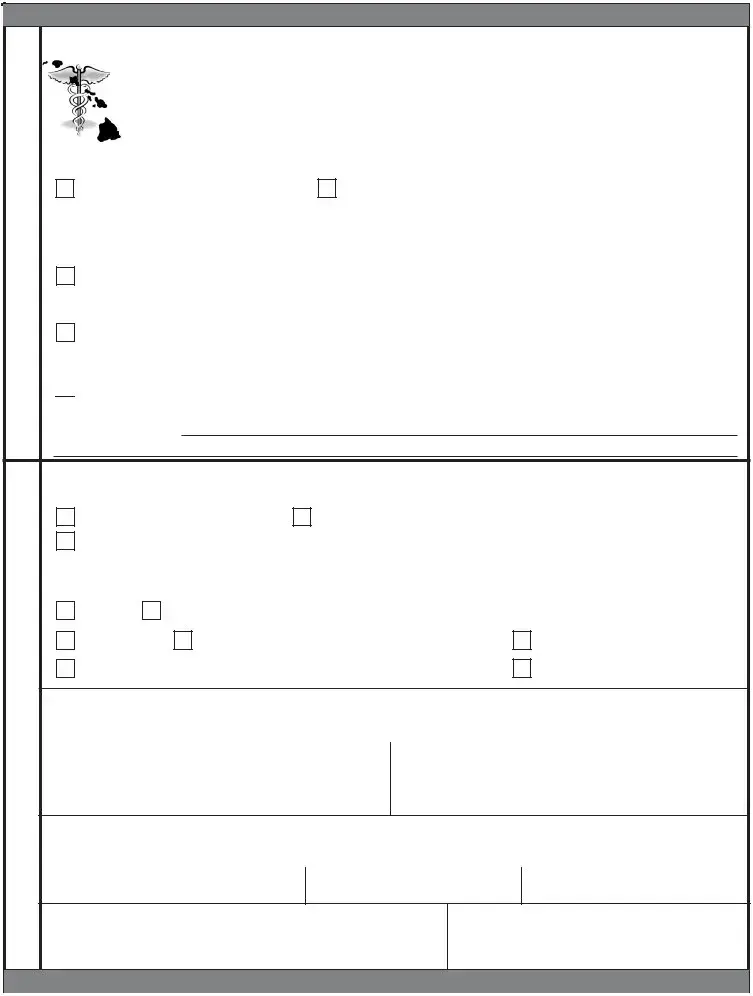
HIPAA PERMITS DISCLOSURE OF POLST TO OTHER HEALTH CARE PROFESSIONALS AS NECESSARY
PROVIDER ORDERS FOR
|
FIRST follow these orders. THEN contact the |
|
Paient’s Last Name |
|
|
|
paient’s provider. This Provider Order form is |
|
|
|
|
|
based on the person’s current medical condiion |
|
|
|
|
|
|
First/Middle Name |
|
||
|
and wishes. Any secion not completed implies |
|
|
|
|
|
full treatment for that secion. Everyone shall be |
|
|
|
|
|
|
Date of Birth |
Date Form Prepared |
||
|
treated with dignity and respect. |
|
|
||
|
|
|
|
|
|
|
|
|
|||
A |
CARDIOPULMONARY RESUSCITATION (CPR): ** Person has no pulse and is not breathing ** |
||||
Atempt Resuscitaion/CPR |
Do Not Atempt Resuscitaion/DNAR (Allow Natural Death) |
||||
Check |
(Secion B: Full Treatment required) |
|
|
|
|
One |
|
|
|
|
|
If the paient has a pulse, then follow orders in B and C. |
|
||||
|
|
||||
B |
MEDICAL INTERVENTIONS: |
|
** Person has pulse and/or is breathing ** |
||
Comfort Measures Only Use medicaion by any route, posiioning, wound care and other measures to relieve pain |
|||||
Check |
and suffering. Use oxygen, sucion and manual treatment of airway obstrucion as needed for comfort. TRANSFER IF COMFORT |
||||
One |
needs cannot be met in current locaion. |
|
|
|
|
Limited Addiional Intervenions Includes care described above. Use medical treatment, anibioics, and IV fluids as indicated. Do not intubate. May use less invasive airway support (e.g. coninuous or
 Full Treatment Includes care described above. Use intubaion, advanced airway intervenions, mechanical venilaion, and defibrillaion/cardioversion as indicated. TRANSFER to hospital if indicated. Includes intensive care.
Full Treatment Includes care described above. Use intubaion, advanced airway intervenions, mechanical venilaion, and defibrillaion/cardioversion as indicated. TRANSFER to hospital if indicated. Includes intensive care.
Addiional Orders:
C |
ARTIFICIALLY ADMINISTERED NUTRITION: Always offer food and liquid by mouth if feasible |
|
|||||
(See Direcions on next page for informaion on nutriion & hydraion) |
and desired. |
|
|||||
Check |
No arificial nutriion by tube. |
Defined trial period of arificial nutriion by tube. |
|
||||
One |
Goal: |
|
|
|
|||
|
|
|
|
|
|
||
|
|
|
|
|
|
||
|
Addiional Orders: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
D |
SIGNATURES AND SUMMARY OF MEDICAL CONDITION - Discussed with: |
|
|||||
Paient or |
Legally Authorized Representaive (LAR). If LAR is checked, you must check one of the boxes below: |
|
|||||
|
|
||||||
Check |
|
|
|
|
|
|
|
Guardian |
Agent designated in Power of Atorney for Healthcare |
|
|||||
One |
|
||||||
|
|
|
|
|
|
|
|
|
Surrogate selected by consensus of interested persons (Sign secion E) |
Parent of a Minor |
|
||||
|
|
|
|
|
|
|
|
Signature of Provider (Physician/APRN licensed in the state of Hawai‘i.)
My signature below indicates to the best of my knowledge that these orders are consistent with the person’s medical condiion and preferences.
Print Provider Name |
Provider Phone Number |
Date |
|
|
|
Provider Signature (required) |
Provider License # |
|
Signature of Paient or Legally Authorized Representaive
My signature below indicates that these orders/resuscitaive measures are consistent with my wishes or (if signed by LAR) the known wishes and/or in the best interests of the paient who is the subject of this form.
Signature (required) |
Name (print) |
Relaionship (write ‘self’ if paient) |
Summary of Medical Condiion
Official Use Only
SEND FORM WITH PERSON WHENEVER TRANSFERRED OR DISCHARGED
HIPAA PERMITS DISCLOSURE OF POLST TO OTHER HEALTH CARE PROFESSIONALS AS NECESSARY
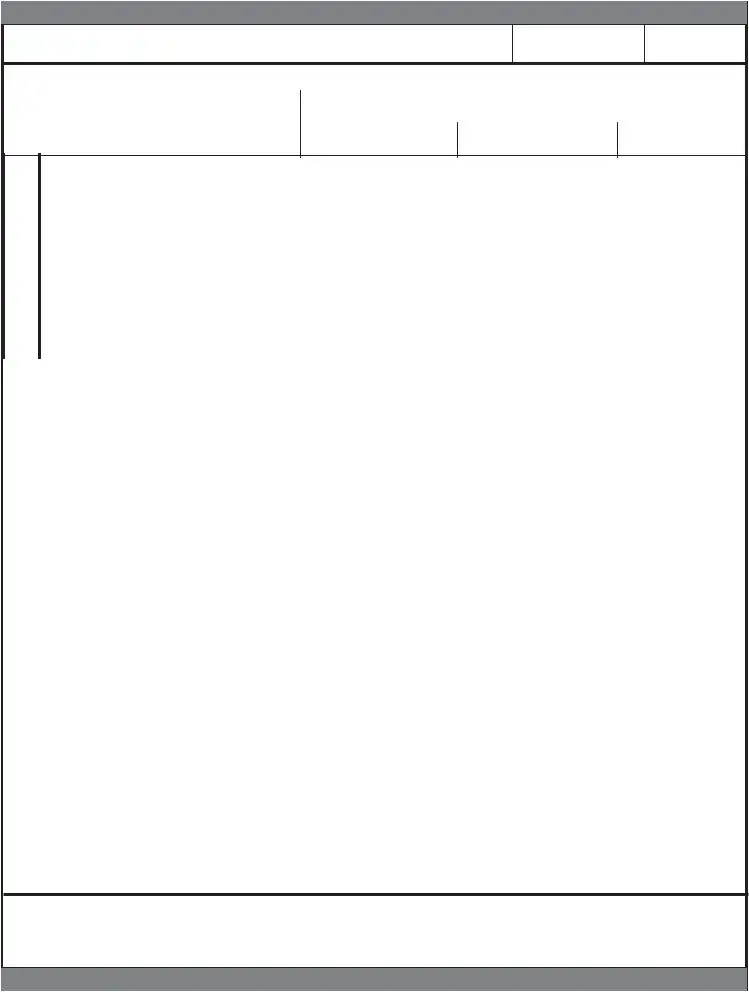
Paient Name (last, first, middle)
Date of Birth
Gender
M F
Patient’s Preferred Emergency Contact or Legally Authorized Representative
Name |
Address |
|
Phone Number |
|
|
|
|
Health Care Professional Preparing Form |
Preparer Title |
Phone Number |
Date Form Prepared |
E |
SURROGATE SELECTED BY CONSENSUS OF INTERESTED PERSONS |
(Legally Authorized Representaive as outlined in secion D) |
|
I make this declaraion under the penalty of false swearing to establish my authority to act as the legally authorized represen- |
|
|
taive for the paient named on this form. The paient has been determined by the primary physician to lack decisional |
capacity and no health care agent or court appointed guardian or
|
Signature (required) |
Name |
Relaionship |
|
|
|
|
Compleing POLST
DIRECTIONS FOR HEALTH CARE PROFESSIONAL
•Must be completed by health care professional based on paient preferences and medical indicaions.
•POLST must be signed by a Physician or Advanced Pracice Registered Nurse (APRN) licensed in the state of Hawai‘i and the paient or the paient’s legally authorized representaive to be valid. Verbal orders by providers are not acceptable.
•Use of original form is strongly encouraged. Photocopies and FAXes of signed POLST forms are legal and valid.
Using POLST
• Any incomplete secion of POLST implies full treatment for that secion. Secion A:
• No defibrillator (including automated external defibrillators) should be used on a person who has chosen “Do Not Atempt Resuscitaion.”
Secion B:
•When comfort cannot be achieved in the current seing, the person, including someone with “Comfort Measures Only,” should be transferred to a seing able to provide comfort (e.g., treatment of a hip fracture).
•IV medicaion to enhance comfort may be appropriate for a person who has chosen “Comfort Measures Only.”
•A person who desires IV fluids should indicate “Limited Intervenions” or “Full Treatment.”
Secion C:
• A paient or a legally authorized representaive may make decisions regarding arficial nutriion or hydraion. However, a surrogate who has not been designated by the paient (surrogate selected by consensus of interested persons) may only make a decision to withhold or withdraw arificial nutriion and hydraion when the primary physician and a second independent physician cerify in the paient’s medical records that the provision or coninuaion of arificial nutriion or hydraion is merely prolonging the act of dying and the paient is highly unlikely to have any neurological response in the future. HRS
Reviewing POLST
It is recommended that POLST be reviewed periodically. Review is recommended when:
•The person is transferred from one care seing or care level to another, or
•There is a substanial change in the person’s health status, or
•The person’s treatment preferences change.
Modifying and Voiding POLST
•A person with capacity or, if lacking capacity the legally authorized representaive, can request a different treatment plan and may revoke the POLST at any ime and in any manner that communicates an intenion as to this change.
•To void or modify a POLST form, draw a line through Secions A through E and write “VOID” in large leters on the original and all copies. Sign and date this line. Complete a new POLST form indicaing the modificaions.
•The paient’s provider may medically evaluate the paient and recommend new orders based on the paient’s current health status and goals of care.
Kōkua Mau – Hawai‘i Hospice and Palliaive Care Organizaion
Kōkua Mau is the lead agency for implementaion of POLST in Hawai‘i. Visit www.kokuamau.org/polst to download a copy
or find more POLST informaion. This form has been adopted by the Department of Health July 2014
Kōkua Mau • PO Box 62155 • Honolulu HI 96839 • info@kokuamau.org • www.kokuamau.org
SEND FORM WITH PERSON WHENEVER TRANSFERRED OR DISCHARGED
Document Characteristics
| Fact | Description |
|---|---|
| Legal Basis | The Hawaii POLST form operations are guided by the Hawaii Revised Statutes §327E-5, specifically for decisions about artificial nutrition and hydration. |
| Form Completion Requirements | The POLST must be completed by a healthcare professional based on patient preferences and medical indications. It requires signatures from either a physician or an Advanced Practice Registered Nurse (APRN) licensed in Hawaii and the patient or their legally authorized representative. |
| Validity of Copies | Original forms are recommended for use, but photocopies and faxes of signed POLST forms are considered legal and valid. |
| Decision Making for Artificial Nutrition | A patient or legally authorized representative can make decisions regarding artificial nutrition or hydration. A surrogate not designated by the patient can make decisions to withhold or withdraw artificial nutrition and hydration only under specific conditions certified by the primary physician and a second independent physician. |
| Review and Modification | POLST forms should be reviewed when the patient is transferred, there's a substantial change in health status, or the patient's treatment preferences change. They can be voided or modified by the patient or legally authorized representative at any time, requiring a new form for changes. |
Guidelines on Utilizing Hawaii Polst
The Hawaii POLST (Provider Orders for Life-Sustaining Treatment) form is a crucial document intended for individuals facing serious health conditions, enabling them to outline their preferences for life-sustaining treatments. Created in collaboration between patients and their healthcare providers, this form ensures that medical treatment aligns closely with the patient's wishes, particularly in emergency situations where the individual might not be able to communicate their decisions. Here are the steps required to fill out the form effectively.
- Begin by filling out the patient's last name, first name, middle name, and date of birth at the top of the form to ensure it is matched correctly with the patient’s medical records.
- Under the Date Form Prepared section, note the date when the POLST form is being filled out.
- In section A, indicate the patient’s preference for cardiopulmonary resuscitation (CPR) should the individual have no pulse and not be breathing. Check the appropriate box for either attempting resuscitation (CPR) or not (Do Not Attempt Resuscitation/DNAR).
- Section B asks for a decision on the level of medical interventions desired. Options range from comfort measures only, to limited additional interventions, up to full treatment, including intubation and mechanical ventilation if needed. Mark the selection that aligns with the patient’s wishes.
- For section C, decide on the approach towards artificially administered nutrition, such as through a feeding tube. Options include not using artificial nutrition, opting for a defined trial period, or selecting long-term artificial nutrition. Check the box that reflects the patient’s preferences.
- The section labeled D SIGNATURES AND SUMMARY OF MEDICAL CONDITION must be completed to validate the POLST form. It involves discussions with either the patient or the patient’s legally authorized representative (LAR). Indicate whom the form was discussed with and check the appropriate box reflecting their relationship to the patient. The healthcare provider must then sign, print their name, provide their phone number and license number, and indicate the date.
- Where applicable, the patient or LAR must sign and print their name, stating their relationship to the patient, to confirm that the orders are in accordance with the patient’s wishes or best interests.
- For patients lacking decisional capacity, without a previously designated LAR, section E allows for the selection of a surrogate by consensus. The selected surrogate must read this section carefully, understanding the limitations regarding decisions to withhold or to withdraw artificial hydration and nutrition, then sign and print their name and relationship to the patient.
- Review instructions provided for both the healthcare professional preparing the form and general guidelines about using the POLST to ensure all information is accurately represented and understood.
Remember, the POLST form accompanies the patient whenever they are transferred or discharged and is a critical component of communicating a patient’s healthcare preferences across different care settings. It’s recommended that the POLSТ form be reviewed periodically, especially when a patient's health status or treatment preferences change. This proactive approach supports the delivery of care that is consistent with the patient's desires, respecting their dignity and rights at all times.
Understanding Hawaii Polst
FAQs About the Hawaii POLST Form
- What is a POLST form and who should have one?
A POLST (Provider Orders for Life-Sustaining Treatment) form is a medical order that outlines a patient's preferences for medical treatment, specifically concerning life-sustaining treatments. It is designed for individuals with serious health conditions or those who are at the end of their life. The Hawaii POLST form helps ensure that healthcare professionals are aware of and respect the patient's wishes regarding treatments like CPR (cardiopulmonary resuscitation), medical interventions, and artificially administered nutrition. This form is recommended for individuals whose healthcare provider believes they might be at risk for a medical emergency where they cannot speak for themselves.
- How is a POLST form different from an advance directive?
While both POLST forms and advance directives are used to communicate a patient's wishes regarding medical treatment, they serve different purposes and are used at different stages of healthcare planning. An advance directive is a legal document that an individual fills out before any medical emergency occurs, designating a healthcare agent and outlining general wishes about life-sustaining treatment. In contrast, a POLST form is a medical order that is completed by a healthcare professional based on conversations with the patient or the patient's legally authorized representative about more immediate treatment decisions in light of the patient's current medical condition. Unlike advance directives, POLST forms are intended for those who are already seriously ill or at the end of life.
- What happens if a section of the POLST form is left incomplete?
If any section of the Hawaii POLST form is not filled out, it is assumed that the patient prefers to receive full treatment for that particular type of care. This implies that in the absence of specific orders, medical professionals will proceed with all treatments necessary to sustain the patient's life. This approach ensures that the patient's care preferences are followed as closely as possible, even if the form is not fully completed.
- Can a POLST form be changed or revoked after it’s been completed?
Yes, a POLST form can be modified or completely revoked at any time by the patient or their legally authorized representative. To void or modify the form, a line should be drawn through sections A through E, and "VOID" should be written in large letters on the original and all copies of the form. Following this, a new POLST form can be completed with the updated orders. It’s important that anytime a patient's treatment preferences change, the POLST form is reviewed and revised accordingly to reflect those new decisions. This ensures that the patient’s current wishes are always known and can be followed by healthcare providers.
Common mistakes
Completing the Hawai'i POLST form (Provider Orders for Life-Sustaining Treatment) is a crucial step in ensuring that an individual's medical treatment preferences are followed, especially during critical times. However, it is common for some to make errors during this process. Recognizing these mistakes can be pivotal in ensuring the document reflects true wishes and is legally compliant.
Not discussing the form with a healthcare provider: The POLPLookingfessional based on the patient's preferences and medical indications, meaning discussions between the patient and healthcare professionals are paramount for accuracy.
Leaving sections incomplete: Any section that is not completed implies that full treatment desires in that particular area, potentially leading to interventions that the patient might not want.
Failure to update the form after healthcare wishes change: The POLST form should reflect the current care desires of the patient. It necessitates revisions whenever there's a substantial change in the person’s health status or they alter their treatment preferences.
Misunderstanding the sections regarding artificially administered nutrition: Decisions about artificial nutrition or hydration can be complex and require clear understanding and precise instructions on the form to ensure the patient's wishes are followed.
Not involving legally authorized representatives when indicated: Especially in cases where the patient lacks decisional capacity, it is crucial to have the form signed by a patient or their legally authorized representative to ensure validity.
Using unclear handwriting or not using blue or black ink: For the document to be legal and valid, including being understood by all healthcare professionals who may read it, clarity and the use of appropriate ink are important.
Not correctly indicating the decision about cardiopulmonary resuscitation (CPR): The form clearly distinguishes between attempting resuscitation and not attempting resuscitation (DNAR - Do Not Attempt Resuscitation), and an incorrect indication can lead to undesired outcomes.
Omitting required signatures and dates: For a POLST form to be executed legally, it must be signed and dated by the provider as well as the patient or the legally authorized representative.
Avoiding these miyetakes not only ensures that the POLST form is legally compliant but also securely reflects the patient's treatment preferences, providing peace of mind to all involved.
Documents used along the form
When dealing with the sensitive and paramount issue of life-sustaining treatment, particularly in Hawaii, the Provider Orders for Life-Sustaining Treatment (POLST) form serves as a vital tool in ensuring that a patient's wishes are respected and adhered to. This form, crucial in its capacity, often works in conjunction with several other documents and forms to provide a comprehensive approach to end-of-life planning. These documents not only facilitate clear communication between healthcare providers and patients but also ensure that the legal and personal aspects of a patient's wishes are fully documented and easily accessible.
- Advance Health Care Directive (AHCD): This legally binding document allows an individual to detail their preferences for medical treatment in the event that they become unable to communicate or make decisions for themselves. It often includes the appointment of a health care proxy or power of attorney who is authorized to make health care decisions on the individual's behalf.
- Durable Power of Attorney for Healthcare (DPOA-HC): Similar to the AHCD, this document specifically grants an appointed individual the authority to make all types of health care decisions, not just those involving life-sustaining treatment, on behalf of the incapacitated individual. It becomes effective only under the circumstances outlined in the document.
- Living Will: A living will is a written, legal document that specifies the types of medical treatments and life-sustaining measures an individual wishes or does not wish to receive if they're unable to communicate. These can include preferences on the use of ventilators, resuscitation, and artificial hydration and nutrition.
- Do Not Resuscitate (DNR) Order: This medical order is signed by a physician and instructs healthcare providers not to perform cardiopulmonary resuscitation (CPR) if the patient's breathing stops or if the patient's heart stops beating. It is more limited in scope than a POLST and is specifically aimed at the event of cardiac or respiratory arrest.
- Medical Orders for Scope of Treatment (MOST): Similar to a POLST, this is a doctor's order that specifies the types of medical treatment an individual wishes to receive towards the end of life. While not available in all states, it covers preferences regarding CPR, medical interventions, antibiotics, and artificially administered nutrition and hydration.
Collectively, these documents play an integral role in end-of-life care planning. They ensure that the healthcare team understands the patient's wishes fully, respects their autonomy, and provides care that aligns with their values and preferences. Incorporating these documents into the patient's care plan promotes a patient-centered approach to treatment, enhances communication among caregivers, and supports legal and ethical decision-making processes.
Similar forms
The Hawaii POLST form is similar to other documents designed to guide healthcare treatments according to a patient's wishes. One such document is the Advance Directive. Like the POLST, an Advance Directive outlines a patient’s preferences for medical treatment and interventions. However, they serve slightly different purposes and are used in different contexts. An Advance Directive is broader in scope, allowing individuals to articulate their values and preferences in more detail, including end-of-life care, and typically comes into play when the patient is unable to make decisions. It can include the appointment of a healthcare proxy or power of attorney for healthcare decisions. In contrast, the POLST is a medical order that translates these preferences into actionable medical orders for those with serious illnesses or at the end of life, making it immediately actionable by healthcare professionals.
Another document similar to the Hawaii POLST form is the Do Not Resuscitate (DNR) order. Both the POLST and DNR orders guide emergency medical personnel on whether to perform CPR or other life-sustaining treatments when a patient’s heart stops or they stop breathing. The key difference lies in their scope. A DNR is specifically focused on the non-performance of CPR, while the POLST covers a broader range of treatments and interventions beyond CPR, such as intubation, mechanical ventilation, and artificially administered nutrition. Additionally, the POLST includes options for less invasive interventions and outlines treatment goals for both emergency and non-emergency situations.
Dos and Don'ts
When filling out the Hawaii Provider Orders for Life-Sustaining Treatment (POLST) form, it is important to ensure that the intentions and medical wishes of either you or your loved one are clearly communicated. Here are some guidelines on what you should and shouldn't do during the process:
- Do ensure the form is completed by a qualified health care professional, as it must be based on patient preferences and medical indications.
- Do make sure the POLST form is signed by both the patient or the patient’s legally authorized representative (LAR) and a physician or Advanced Practice Registered Nurse (APRN) licensed in the state of Hawaii for it to be valid.
- Do review and discuss all treatment options thoroughly with the health care provider to ensure that the decisions made reflect the patient's wishes.
- Do remember to send the form with the patient when they are transferred or discharged to any other care setting.
- Don't leave any section incomplete unless you wish to imply full treatment for that section. Incompleted sections are interpreted as a preference for full treatment.
- Don't use verbal orders for the POLST form – it must be documented and signed on the actual form to be legally valid. Verbal preferences need to be translated into written orders on the form.
- Don't forget to review and potentially update the POLST form if the patient's health status or treatment preferences change, especially upon transfer to a new care setting or a significant change in health condition.
- Don't hesitate to void or modify the form if treatment wishes change. To do this, simply draw a line through the sections A through E, write "VOID" in large letters, sign, and date it. Then, fill out a new POLST form to reflect the current wishes.
Understanding and respecting these guidelines will help ensure the POLST form accurately reflects the patient's wishes regarding life-sustaining treatment and is properly adhered to by health care providers.
Misconceptions
There are several misconceptions about the Hawaii Provider Orders for Life-Sustaining Treatment (POLST) form that deserve clarification to ensure individuals and families are well-informed about their healthcare decisions. Below are six common misunderstandings and the truths behind them:
Only the elderly or those with a terminal illness need a POLST form. In reality, the POLST form is designed for anyone with a serious illness or frail condition, regardless of their age. It's a tool to communicate their treatment preferences effectively.
A POLST form is legally binding across all states. While many states have a form of POLST, the recognition and specific legislation surrounding it can vary. The Hawaii POLST is specifically designed according to Hawaii's laws and may not be recognized in the same manner in other states.
Completing a POLST form means you’re refusing all treatment. This is not the case. The POLST form enables individuals to make decisions about the types of life-sustaining treatment they do or do not want. This can include full treatment, limited interventions, or comfort-focused care.
If you change your mind, the POLST form cannot be altered. Patients or their legally authorized representatives can update their POLST form whenever their preferences or conditions change. It's important to communicate any changes to healthcare providers immediately.
The POLST form is the same as a Last Will and Testament. A POLST form is not the same as a will. A will deals with estate and personal matters after someone's death. In contrast, a POLST form provides medical orders for a healthcare provider to follow while the patient is still alive.
Having a POLST form means you do not need an Advance Health Care Directive. Actually, these two documents serve different purposes and work best in conjunction. The Advance Health Care Directive appoints a health care agent and outlines general wishes about treatment, while the POLST provides specific medical orders based on those wishes and current medical conditions.
Understanding the facts about the Hawaii POLST form is crucial for making informed healthcare decisions tailored to personal values and medical conditions. It is always recommended to discuss with healthcare providers to ensure the document accurately reflects one's wishes.
Key takeaways
The Hawaii POLST (Provider Orders for Life-Sustaining Treatment) form is a critical legal document designed to ensure that a person's wishes regarding medical treatment are honored, particularly towards the end of life. Understanding its key aspects is essential for both individuals and their families. Here are nine key takeaways about filling out and using the Hawaii POLST form:
- The POLST form must be completed by a healthcare professional (a physician or Advanced Practice Registered Nurse licensed in Hawaii) based on the patient's current medical condition and personal desires, ensuring the instructions are clear and reflective of the patient’s wishes.
- All sections of the POLST form that are not completed imply that full treatment should be provided in those areas. This ensures that no assumptions are made regarding a patient's preferences for care.
- Section A of the form addresses cardiopulmonary resuscitation (CPR) and differentiates between attempting resuscitation and do not attempt resuscitation (DNAR), explicitly instructing healthcare providers on the action to take should the patient's heart stop.
- Section B focuses on medical interventions beyond CPR, detailing the extent of treatments desired, from full treatment, including the use of intubation and mechanical ventilation, to comfort measures only, emphasizing pain relief and comfort rather than extending life.
- In Section C, decisions regarding artificially administered nutrition offer choices from not using artificial means of nutrition to long-term artificial nutrition, providing clear directives about the patient’s wishes on sustenance if unable to feed themselves.
- The form requires signatures from both the healthcare provider and the patient or the patient’s legally authorized representative (LAR), verifying that the orders align with the patient’s medical condition and wishes, ensuring a legally binding document.
- Verbal orders are not acceptable; the POLST form must be signed by the designated medical professionals and the patient or LAR to be valid, emphasizing the importance of documented consent.
- The form should be reviewed periodically, especially when the person’s healthcare setting, health status, or treatment preferences change, ensuring the POLST remains relevant and reflective of the current wishes and medical condition.
- It is possible to modify or void the POLST form if the patient’s wishes change. This can be done by the patient or their LAR by drawing a line through the sections A-E, writing "VOID," and completing a new POLST form with the adjusted preferences.
In summary, the Hawaii POLST form acts as a bridge between a patient's healthcare preferences and the actual medical care received, particularly in emergency situations or towards the end of life. It's a vital document that requires careful discussion and completion to accurately reflect the patient's wishes, ensuring they are respected by healthcare providers.
Create Common PDFs
Hawaii State Tax Forms - Businesses conducting transactions subject to general excise tax or use tax in Hawaii need to file this form.
G-17 Form - The G-17 form plays a pivotal role in the documentation and regulation of tax-exempt transactions within Hawaii’s commercial landscape.
Hawaii Llc Cost - Form X-8 filing is part of regulatory compliance for businesses operating in Hawaii.